The Fragmented Landscape of Healthcare Data: Why Integration Is No Longer Optional
Walk into any modern hospital, and you’ll see connected devices, digital dashboards, and clinicians glued to their EHRs. On the surface, healthcare appears to be digitized. However, dig deeper, and you’ll uncover a sobering truth: our data still resides in silos, scattered across systems, organizations, and formats that don’t communicate with each other.
This isn’t just a technical inconvenience. It’s a strategic and clinical crisis, one that touches every corner of healthcare delivery, from patient safety to population health to payer efficiency.
In this blog, we delve into the persistent issue of data fragmentation, its staggering cost to the system, and most importantly, why meaningful integration is not just a choice, but a pressing need that demands our immediate attention.
The Reality of Fragmentation: A Digital Tower of Babel
Healthcare generates more data than any other industry, accounting for approximately 30% of the world’s total data, according to RBC Capital Markets. This data is expected to grow at a 36% compound annual growth rate, fueled by electronic health records (EHRs), wearables, remote patient monitoring, claims data, genomics, and social determinants of health.
But here’s the paradox: 90% of that data goes unused for care decision-making.
- Hospital and clinic EHRs
- Insurance claims and authorization systems
- Imaging systems (PACS)
- Pharmacy records
- Lab databases
- Devices and IoT sensors
- Public health registries
- Consumer health apps and wearables
These systems communicate in different languages, such as HL7 v2, FHIR, X12, and CCD, and adhere to inconsistent standards and data models. Even within the same hospital network, data exchange can be challenging if different departments use different vendors.
The result? A digital Tower of Babel, where every system has a voice, but no one understands each other.
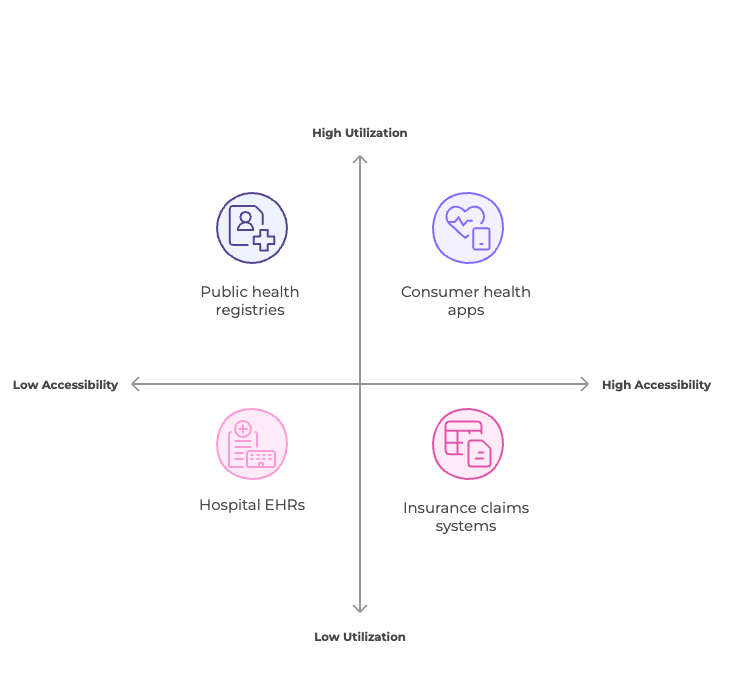
fig: Data Utilization & Accessibility
The Cost of Doing Nothing
1. Redundant Tests and Procedures
Imagine a patient visiting multiple providers, each repeating the same blood test or MRI because previous results aren’t accessible. This isn’t rare, it’s routine.
The National Library of Medicine estimates that $200 billion is wasted annually in the U.S. alone on unnecessary services, many of which stem from inaccessible data.
2. Patient Harm from Medical Errors
When providers lack a comprehensive picture, they make decisions based on incomplete information. This leads to:
- Incorrect medications
- Missed allergies
- Delayed or duplicate treatments
According to a BMJ study, medical errors are the third leading cause of death in the U.S., with data gaps being a major contributor.
3. Provider Burnout and Inefficiency
Clinicians spend up to 6 hours per day managing EHRs, much of which is spent trying to locate, reconcile, or verify information scattered across various systems (Annals of Internal Medicine).
The result is cognitive overload, reduced face time with patients, and escalating burnout, leading to workforce attrition, lower morale, and worse patient outcomes.
4. Lost Revenue and Strategic Risk
For payers, fragmented data results in poor risk stratification, inaccurate quality reporting, and a limited ability to manage value-based care. It undermines HEDIS scoring, Star ratings, and CMS reporting.
For health systems, the inability to track performance, spot care gaps, or optimize networks weakens their strategic edge.
Why Is Integration So Hard?
Technical Heterogeneity
Different formats (e.g., HL7 v2 vs. FHIR), terminologies (SNOMED, ICD, LOINC), and transport protocols make point-to-point integration brittle and unsustainable at scale.
A recent review in the National Library of Medicine outlines how inconsistent schema structures, differing update cycles, and a lack of semantic alignment create barriers even in relatively well-digitized systems.
Privacy and Compliance
Data sharing must comply with HIPAA, GDPR, and regional data governance frameworks. Integration requires handling consent, encryption, auditing, and access controls—all without impacting performance.
The average cost of a healthcare data breach now stands at $10.93 million, the highest across industries (IBM Cost of a Data Breach Report).
Human and Organizational Factors
- Staff fear of workflow disruption
- Vendor lock-in from proprietary systems
- Misaligned incentives (e.g., fee-for-service models that don’t reward interoperability)
Without a comprehensive change management strategy that addresses these human and organizational factors, even the most advanced integration technology is likely to face insurmountable challenges.
So What Works? Building Blocks of Effective Integration
1. Adoption of Open Standards (FHIR, HL7)
Fast Healthcare Interoperability Resources (FHIR) has emerged as the most promising standard for healthcare interoperability. Supported by SMART apps, bulk data exchange, and CMS mandates, FHIR enables:
- Patient-level APIs
- Bulk population data pulls
- App-level interoperability within EHRs
2. Middleware and Interoperability Layers
3. Cloud-native Data Platforms
4. Federated and Edge-based Models
Rather than moving sensitive data across networks, federated learning allows multiple institutions to train models collaboratively without sharing raw data—a critical advancement in privacy-conscious analytics (Nature Machine Intelligence).
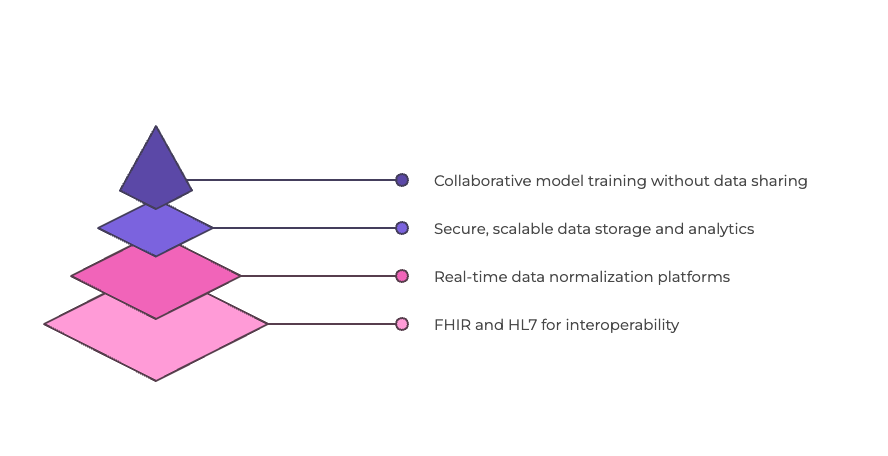
fig: Healthcare Integration Hierarchy
Real-World Example: The UK's Interoperability Dilemma
Final Thoughts: A Call to Act
Healthcare doesn’t need more dashboards, more sensors, or more apps.
It requires connected intelligence, clean, complete, and context-aware data that flows across boundaries, augmenting human decision-making and aligning stakeholders around patient value.
Integration isn’t just an IT initiative. It’s the foundation for every transformative healthcare vision:
- Value-based care
- Precision medicine
- Predictive AI
- Whole-person care models
- Interoperable public health infrastructure
If you’re a payer, a provider, or a product leader in health tech—the time to invest in integration is now. Because when systems don’t talk, patients suffer, providers burn out, and money is wasted.
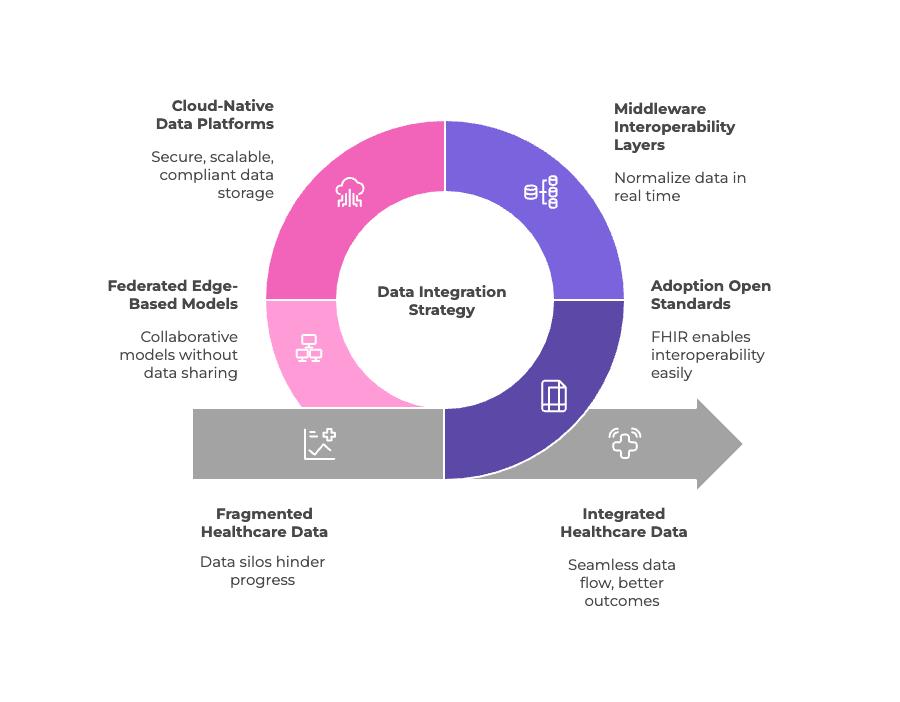
fig: Achieving HealthData Integration
