How Healthcare APIs Are Driving the Future of Interoperability
Over the last decade, healthcare has experienced a surge in digital systems—from electronic health records (EHRs) and radiology information systems to telehealth platforms and payer systems. Yet, ironically, the very abundance of these digital tools has compounded a long-standing problem: data fragmentation.
The average hospital system in the U.S. today runs over 16 disparate IT systems, each with its own data model, integration style, and interface. These systems do not talk to each other easily. The result? Care delays, clinician burnout, billing inefficiencies, and a patient experience that often feels like an administrative obstacle course.
But there is light at the end of the tunnel—Healthcare APIs (Application Programming Interfaces) are rapidly becoming the glue that connects this fragmented ecosystem. At the forefront of this revolution is FHIR® (Fast Healthcare Interoperability Resources)—a modern, web-native standard that IT specialists are instrumental in implementing, designed to make healthcare data accessible, modular, and scalable.
This blog delves into how APIs, powered by standards like FHIR, are transforming interoperability, unlocking the full value of healthcare data, and paving the way for a future of intelligent, patient-centric, and seamless care.
What Are Healthcare APIs, Really?
At its core, an API is a contract between systems: “If you give me a request in this format, I will give you a response.” APIs abstract away the complexity of the underlying system, allowing developers and systems to interact with healthcare data without needing to know its storage, structure, or source.
In the healthcare context, APIs:
- Enable EHRs to share data with labs, pharmacies, payers, and external apps
- Power patient-facing tools like mobile health apps, wearables, and personal health records
- Support clinical workflows like prior authorizations, care coordination, and referral management
- Provide structured data access to enable dashboards, analytics, and AI engines
The HL7® FHIR standard—developed by Health Level Seven International—is now the global benchmark for how these APIs should be built in healthcare.
The Rise of FHIR: Why It’s a Game-Changer
FHIR isn’t just another standard—it’s the first healthcare interoperability standard purpose-built for the web era. While older standards, such as HL7 v2 and CDA, relied on XML-heavy, message-based designs, FHIR is RESTful, lightweight, and flexible. It uses familiar web technologies:
- HTTP methods (GET, POST, PUT, DELETE)
- JSON and XML for payloads
- OAuth2 and SMART on FHIR for authentication
This makes FHIR not only easy to adopt but also extremely developer-friendly—opening the doors for innovation from startups, enterprise vendors, payers, and health systems alike.
Real-World ROI: Where Healthcare APIs Are Making an Impact
The promise of APIs is not just theoretical; it is a reality. Across the globe, APIs are demonstrating tangible outcomes:
Boston Children's Hospital
Used FHIR APIs to unify pediatric patient data across departments, resulting in:
- 25% reduction in IT overhead
- Faster access to diagnostics across departments
- Enhanced patient satisfaction with seamless care navigation
(Source)
MultiCare Health System & Regence
Adopted Da Vinci Project’s FHIR-based “Trebuchet” implementation for prior authorization:
- Reduced turnaround time by 140%
- Replaced cumbersome fax-based processes with real-time eligibility checks and prior auth submissions
- Reduced administrative burden on clinical staff
Intermountain Healthcare
Leveraged APIs to support population health and research coordination:
- Lowered research costs by 15%
- Improved data quality for chronic disease registries
- Enabled near real-time cohort identification for clinical studies
Use Cases Where APIs Are Driving Change
| Use Case | Impact |
|---|---|
| Prior Authorizations | Real-time decisioning slashes wait times from days to minute |
| Medication Reconciliation | Reduced medication errors by up to 70% via FHIR-based medication history |
| Patient Access | Empowered millions of patients to download records via Apple Health, MyChart, etc. |
| Value-Based Care Analytics | Structured APIs enable the measurement of cost, quality, and outcomes at the population scale. |
Global Surge in Adoption
The adoption of APIs, particularly FHIR-based ones, is accelerating worldwide:
- U.S. ONC/CMS Mandates: As of 2021, federal rules mandate that payers and providers expose patient data using FHIR-based APIs
- Australia & New Zealand: FHIR use jumped from 11% to 66% of hospitals in under 5 years
- UK NHS: Has standardized on FHIR as the default for all new API developments, with GP Connect and NHS Digital APIs already live.
Built-in Security & Compliance
Security has historically been a barrier to open data access in the healthcare sector. But modern API protocols overcome this challenge:
- OAuth 2.0 + SMART on FHIR: Granular, role-based access control
- TLS/HTTPS encryption: Ensures end-to-end data protection
- Access logs and audit trails: Meet HIPAA/GDPR compliance mandates
- Scoped tokens: Enable patient-controlled access down to a single FHIR resource (e.g., just their lab results)
📌 APIs now offer not just openness but governed openness—a foundational requirement for interoperable, accountable care.
fig. Governed Openness
Fueling Data Analytics & Clinical Intelligence
APIs make data machine-readable, queryable, and analytics-ready—unlocking opportunities for:
- Dashboards for clinical, operational, and financial KPIs
- Risk stratification and cohort segmentation
- AI-driven prediction models for readmission, sepsis, and disease progression
LLM + FHIR pipelines: GPT models now map unstructured notes to FHIR with >90% accuracy
Architecture Benefits: Scalable, Modular, Cloud-Native
With their stateless, REST-based design, APIs are inherently cloud-native. This means:
- Horizontal scalability: APIs can be deployed in containers and scaled elastically
- Composable services: Each clinical or admin function can be modularized
- Multi-tenant support: Key for payers and platform vendors
- Microservice orchestration: FHIR APIs align well with service meshes and low-code platforms
TechVariable’s accelerators, such as SyncMesh, utilize this design for the dynamic integration of healthcare data across ADT, EHRs, and Claims.
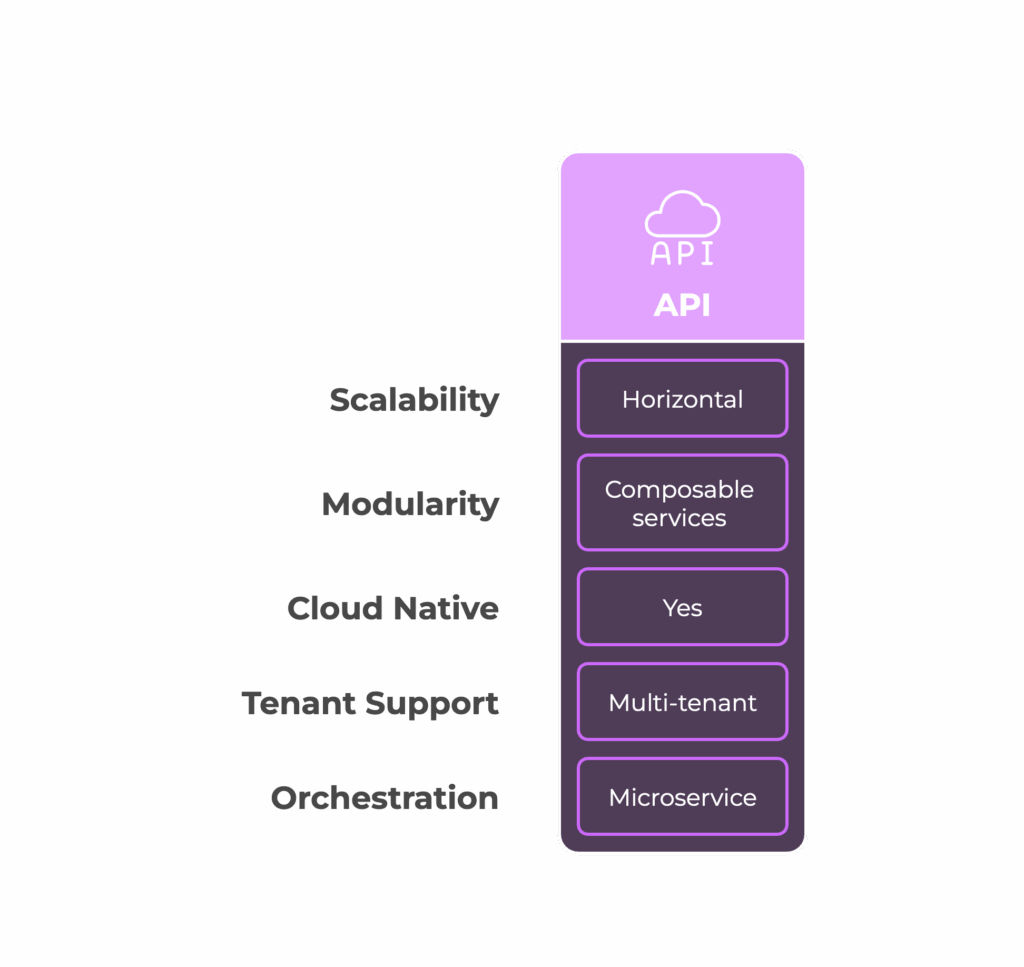
fig. API Architecture Benefits
What’s Holding APIs Back?
Despite widespread enthusiasm, several real-world challenges still need to be addressed:
| Barrier | Details |
|---|---|
| Legacy Systems | Older Electronic Health Records (EHRs) lack native FHIR support, necessitating custom adapters |
| Inconsistent Implementation | Varying interpretations of FHIR resources create "FHIR dialects." |
| Poor Semantic Quality | APIs don't solve data quality issues (e.g., inconsistent codes) |
| Developer Skill Gap | Need for widespread upskilling in API security, HL7, FHIR profiling |
| Cost of Transition | Migration from point-to-point HL7v2 to APIs requires investment and a roadmap. |
These challenges, although non-trivial, are being actively addressed through ecosystem-wide efforts, including the Argonaut Project, the Da Vinci Project, and federal funding incentives.
Future Outlook: APIs + AI + Interoperability = Precision Healthcare
The trajectory is clear: APIs will soon underpin not just interoperability but intelligence in healthcare systems.
- FHIR + AI models will generate contextual nudges for clinicians at the point of care
- APIs will power payer-provider convergence through real-time data sharing
- Patient-owned data will become a reality through universal API access and identity federation
- Composable data platforms will use APIs to integrate third-party modules (LLMs, NLP, imaging analytics, etc.) seamlessly
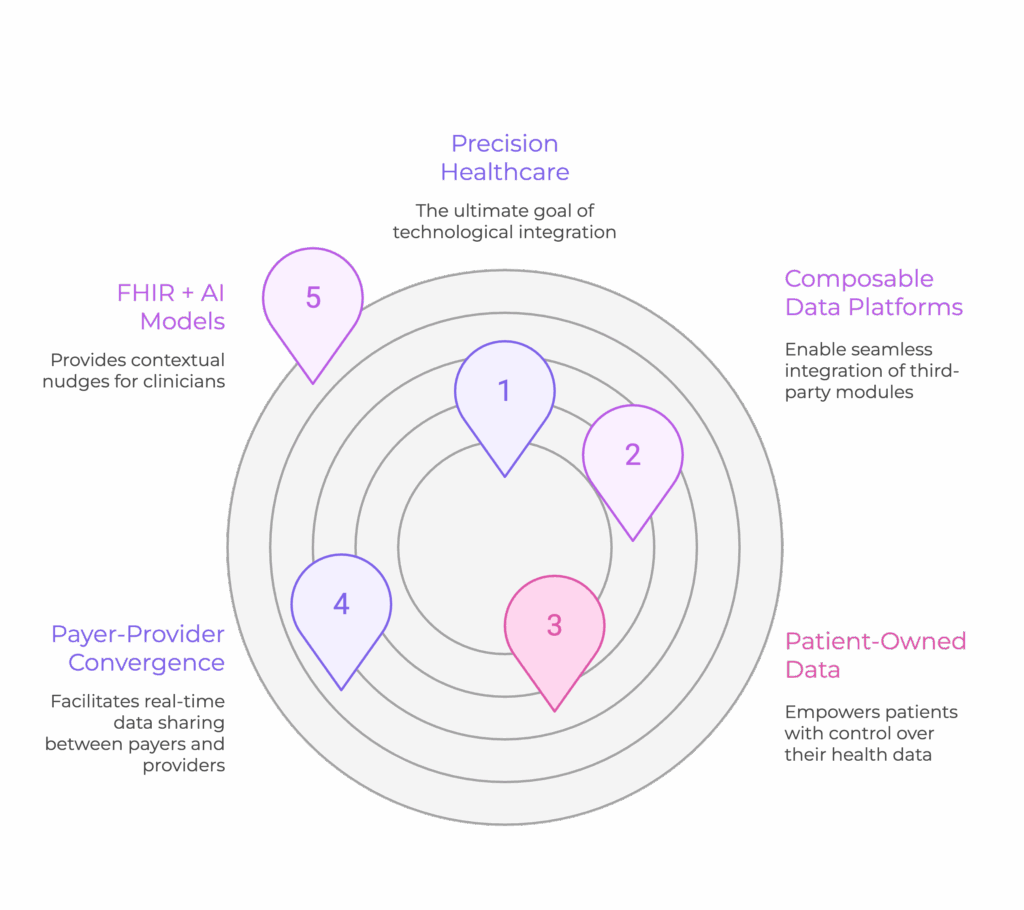
fig. Future Outlook
Final Takeaway: It’s Not Just Technology—It’s Strategy
Healthcare APIs aren’t just a software decision—they’re a strategic shift. They reduce friction, enable innovation, and build a long-term digital foundation for healthcare organizations to:
- Improve care quality and access
- Lower operational costs
- Empower patients and providers
- Compete in a data-first healthcare economy
Whether you’re a provider, payer, or health tech company, your API strategy will determine your future readiness.
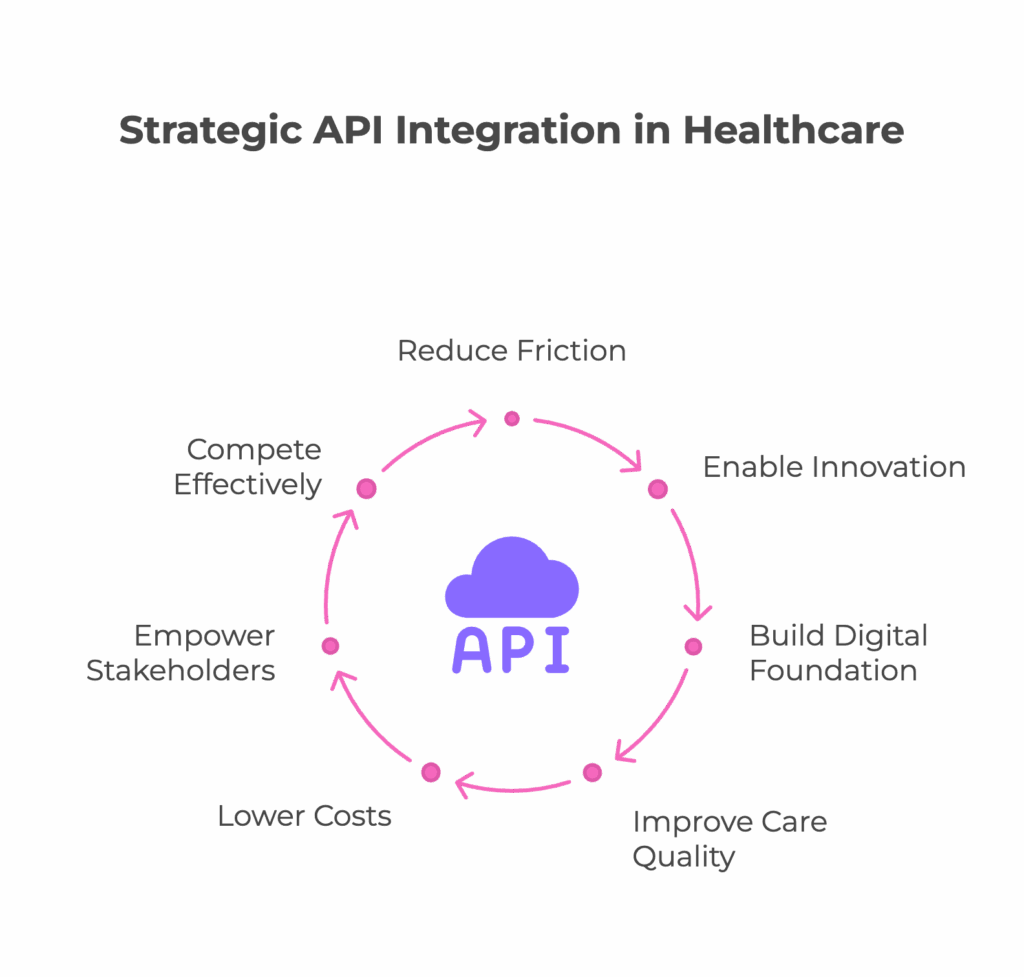
fig. Strategic API Integration in Healthcare



