5 Healthcare Tech Trends Actually Worth Watching in 2026
Look, I’ve been around long enough to see “transformative healthcare trends” come and go. Remember when blockchain was going to revolutionize medical records? Yeah, me too.
But something different is happening now. We’re past the hype cycle on a few key technologies, and they’re starting to actually work. Not in pilot programs or carefully curated demos but in real healthcare settings with real problems. Here’s what I’m seeing that actually matters going into 2026.
1. Longitudinal Patient Records Are Finally Happening (No, Really This Time)
I know, I know. We’ve been talking about this for what, fifteen years? It’s been on every healthcare IT roadmap since the Obama administration. But here’s the thing: it’s actually starting to work now.
What changed? It’s not just that we have better interoperability standards, though FHIR helps. It’s that organizations finally figured out the hard parts: identity matching at scale, getting consent frameworks right, and (this is key) actually putting the data where clinicians need it instead of in some dashboard they’ll never open.
The health systems getting this right aren’t just collecting data from every possible source. They’re building what I’d call “persistent patient graphs,” systems that understand how a patient’s story unfolds over time, across different settings and providers. Clinical notes, claims data, social factors, medication histories, wearable device readings, all of it woven together into something that actually makes sense.
This isn’t just nice to have. It’s becoming the foundation for everything else: better care coordination, accurate risk adjustment, value-based care that actually works. If you’re still thinking episodically in 2026, you’re going to fall behind fast.
Early generative AI in healthcare was basically a fancy chatbot. You’d ask it a question, it would give you an answer, and that was that. Useful? Sometimes. Revolutionary? Not really.
What’s coming in 2026 is different: agentic AI that can observe what’s happening, figure out what needs to be done, and actually do it. We’re talking about systems that will:
- Draft prior auth requests without anyone asking
- Pull together context-rich data and pre-fill forms automatically
- Spot gaps in documentation and fix them before they become problems
- Kick off workflows across multiple systems: your EHR, billing platform, CRM, whatever
I’m seeing pilots right now where these AI agents are cutting manual work by 30-60%. That’s not hype. That’s real time saved. In 2026, expect these pilots to scale up and become standard operating procedure.
The shift is subtle but important: instead of healthcare workers using AI, AI will work alongside them as an actual collaborator. It’s the difference between a tool and a teammate.
3. Making Sense of Healthcare Data (The Boring, Critical Stuff)
Here’s a truth nobody wants to hear: we don’t have a data volume problem anymore. We have a “what does this data actually mean” problem.
Healthcare data is messy. The same condition might be coded three different ways across three different systems. Lab results use different units. Medications have multiple names. And good luck getting claims data to line up with clinical data without a team of analysts and a prayer.
This is where semantic interoperability comes in, and yes, I realize that’s a terrible term. What it really means is using standardized vocabularies (SNOMED CT, RxNorm, LOINC, ICD-10, CPT) to make sure everyone’s speaking the same language.
In 2026, this stops being an analytics problem and becomes an operational necessity. Why? Because all those AI agents I just mentioned? They need clean, standardized data to work safely. And those longitudinal patient records? They’re useless if you can’t accurately interpret what’s in them.
The organizations that figure out their ontology layer (the invisible infrastructure that translates and connects healthcare concepts) will have a massive advantage. The ones that don’t will keep drowning in data they can’t actually use.

4. No-Code Tools for Healthcare Data (Finally)
Remember when you needed a specialized data engineer just to connect two systems? That’s changing fast.
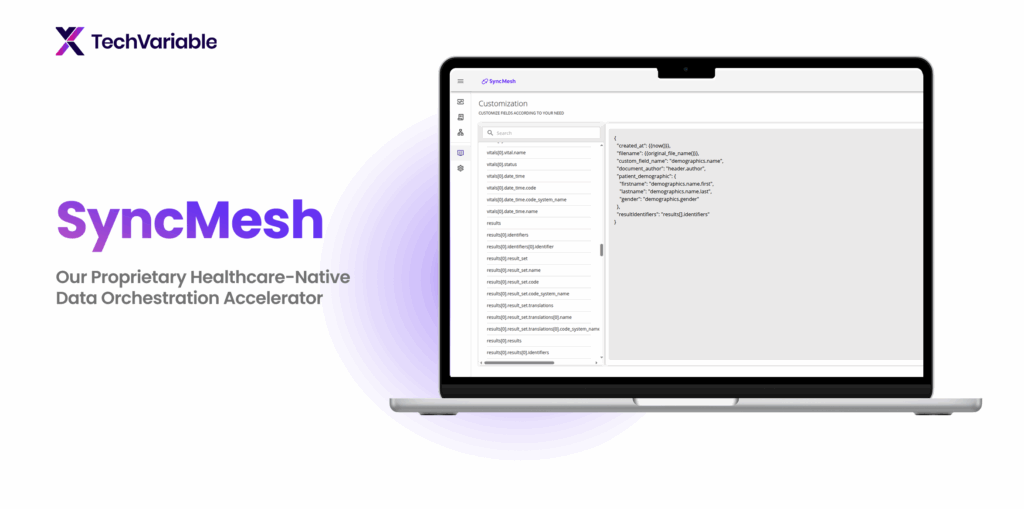
Healthcare organizations are shifting to modular, no-code (or low-code) data platforms that let teams build data pipelines without writing mountains of custom code. Need to pull in a new data feed? It’s configuration, not a six-month development project.
This matters because we’re hitting two problems at once: healthcare data is getting more complex, and there aren’t enough engineers who understand healthcare to go around. No-code platforms solve both.
The good ones come with FHIR data models baked in, handle claims data standardization out of the box, and make compliance workflows actually manageable. You can move fast without breaking things, or more importantly, without breaking HIPAA.
Expect this to accelerate in 2026 as organizations realize they can’t hire their way out of the data engineering shortage.
5. Reducing Clinical Workload Becomes a Measurable Priority
Here’s something you’ll see in boardrooms in 2026: executives tracking clinical workload reduction the same way they track revenue or patient safety metrics.
Why the shift? Because burnout isn’t an HR problem anymore. It’s an operational crisis. We’re short on nurses. We’re short on primary care physicians. Documentation time is out of control. And all of this affects care quality and retention in measurable ways.
But here’s what’s different now: AI-driven automation is making workload reduction actually possible. Not theoretically possible – measurably, quantifiably possible.
Health systems will start tracking things like:
- Documentation time saved per clinician per day
- Reduction in chart review hours
- How many tasks get automated vs. done manually
- Ratio of patient-facing time to administrative work
When boards start measuring something, budget follows. Expect big investments in ambient clinical intelligence, workflow automation, and agentic AI, anything that gives clinicians time back.
What It All Means
These five trends aren’t disconnected. They’re part of a bigger shift from fragmented digital tools to integrated, intelligent healthcare systems. The organizations that get ahead of this, that invest in semantic foundations, workflow automation, and modular data infrastructure now, won’t just lead in 2026. They’ll set the standard for the next decade.
At TechVariable, we’re deep in this work: helping healthcare organizations move from pilots and proofs-of-concept to things that actually scale and work in the real world. Because ultimately, that’s what matters, not what looks good in a demo, but what actually helps patients and makes clinicians’ lives better.
If you’re working on any of this stuff and want to compare notes, reach out. This is too important to get wrong.




