The Hidden Split in Device Enabled Care
Device enabled care generates large volumes of telemetry and encounter data. Yet these records remain in separate systems. Device clouds hold usage logs. EHR systems hold encounters. Payer systems hold claims. This split blocks visibility across the full patient timeline.
How Fragmentation Undermines Clinical Follow Ups
Care teams often lose critical signals. A two week drop in therapy usage may sit inside the device portal, but the EHR does not show it. Without this alignment, coordinators act late. Patients fall out of therapy. This creates care leakage and poor continuity.
The Real Operational Cost
The operational impact is significant.
- Staff copy values from PDFs into EHR fields.
- Teams reconcile timestamps from multiple portals.
- Billing staff correct mismatched codes before submission.
This slows throughput and increases rework on each case.
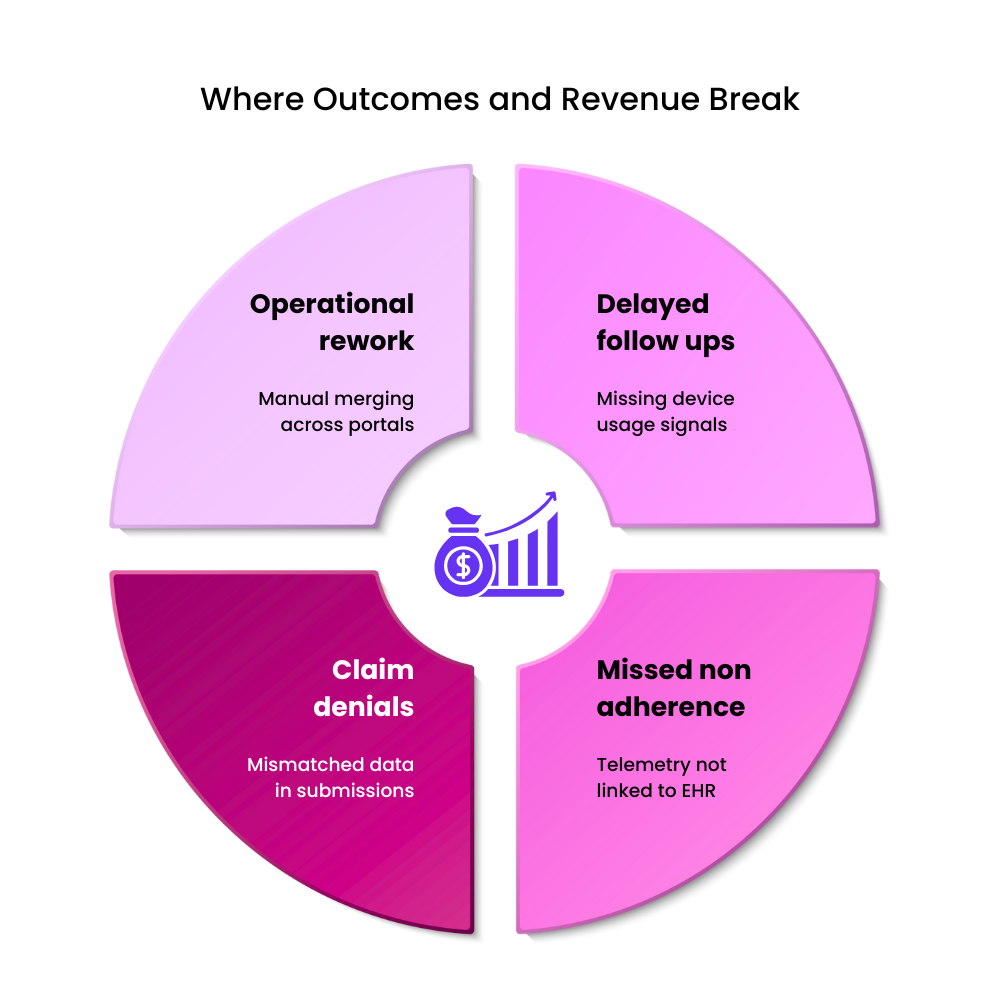
How Fragmentation Affects Revenue
Claims often fail because encounter data, diagnostic codes and usage logs do not match. Payers reject submissions that lack clear linkage between therapy adherence and visit history. This increases denial rates and lengthens reimbursement cycles.
Data Unity as the Turning Point
A unified data layer aligns device telemetry, EHR context and payer events into one record. It reconciles identifiers, timestamps and terminology. Once this foundation exists, teams work from one view. Missed signals drop, reports reach payers on time and claims move with fewer disputes.