2026 Survival Guide: Healthcare Founders Should Avoid These Top 5 Mistakes
Healthcare startups don’t fail because the technology is weak. In 2026, they will fail because the strategy is weak. Because the execution is undisciplined. Because the founder misunderstands how healthcare systems, incentives, and data infrastructures work.
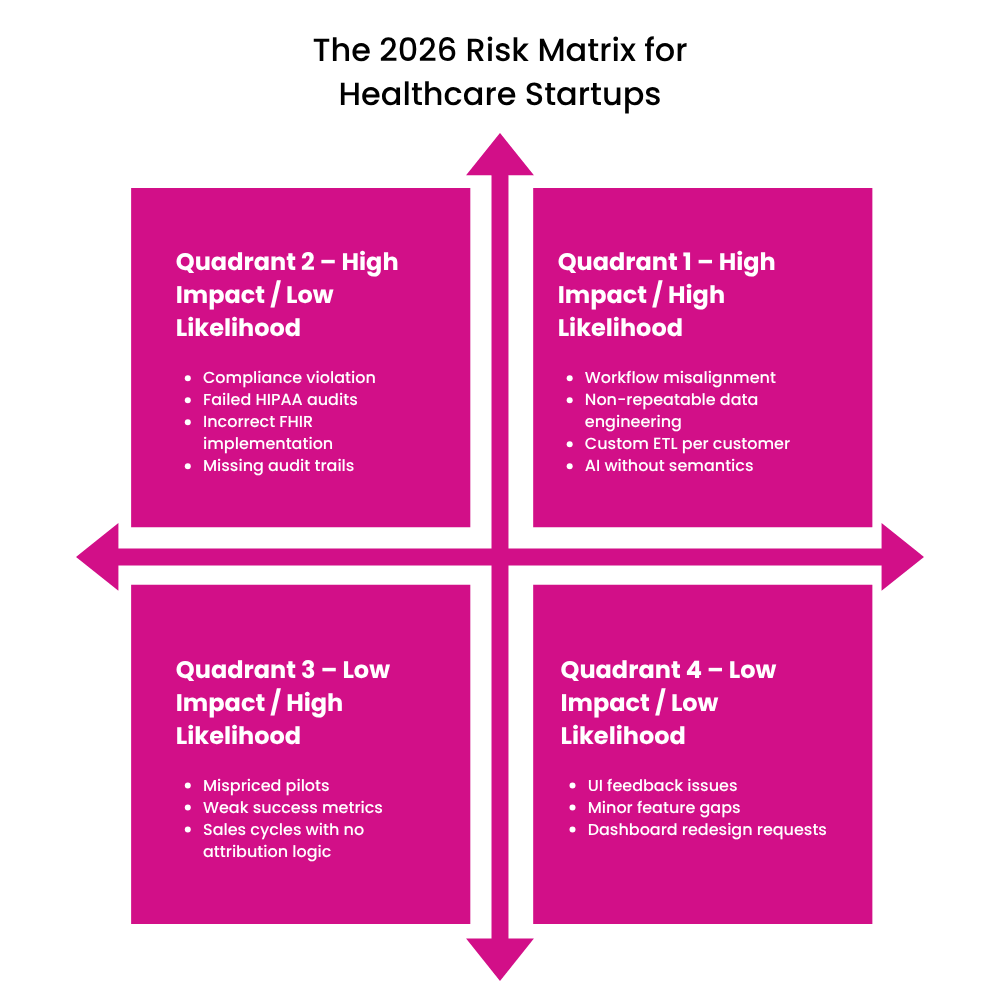
The risks in 2026 won’t be hype or lack of investor appetite. The risks will be the operational killers that derail teams: misjudged interoperability requirements, scoped GTM motions, and solutions that never fit into clinical workflows.
Here are the top 5 mistakes healthcare founders must avoid in 2026, and how planning can keep them out of the danger zone.
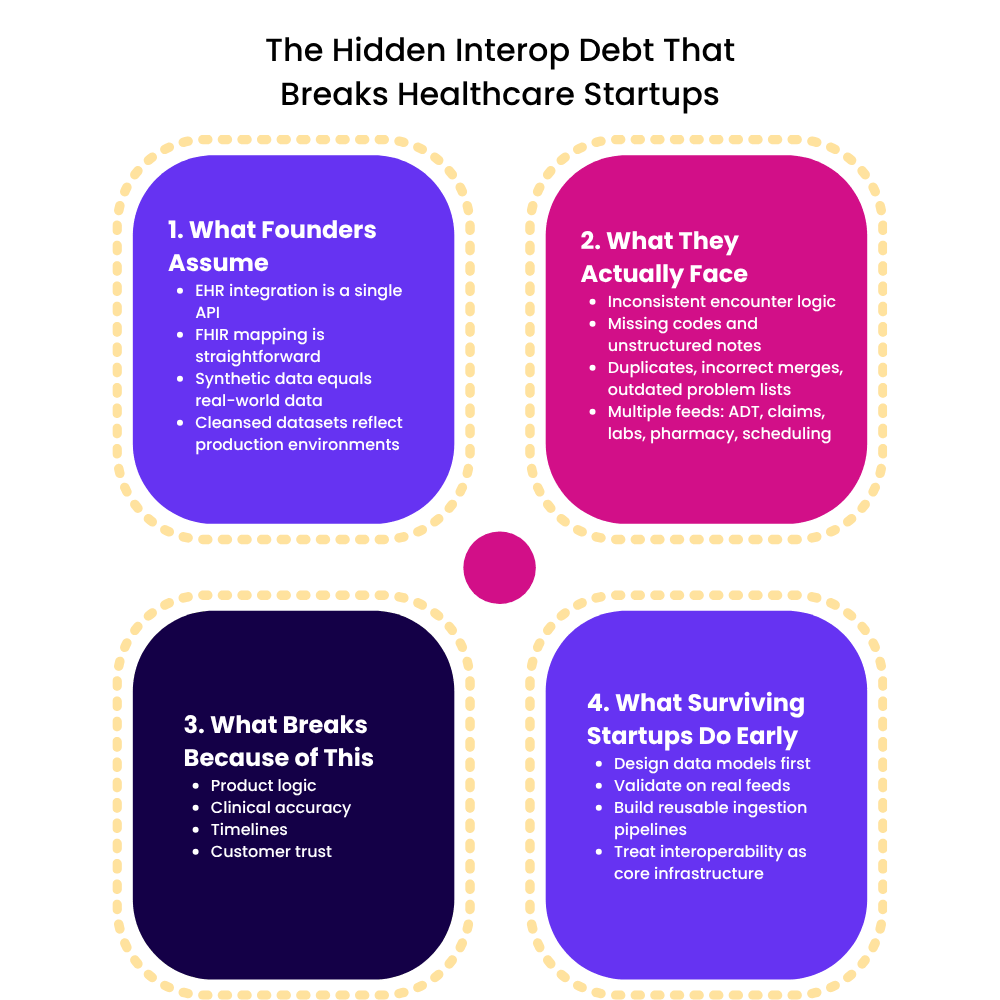
1. Underestimating Interoperability and Data Requirements
Many founders assume, “We’ll integrate with the EHR later.”
But 2026 is the year where “later” becomes too late.
Healthcare systems now expect vendors to show:
- FHIR schemas
- Mappings to ADT, claims, labs, and pharmacy feeds
- Data quality and lineage controls
- Consent, access, and audit tracking
- APIs with version updates
Startups architect for the app, not the data pipelines. Then, when they encounter hospital data (duplicates, missing codes, inconsistent encounter logic), the roadmap collapses.
What I learned:
“A Series A startup once came to us after they had spent 11 months building a product that worked on synthetic data. It broke within 48 hours on hospital feeds. Not because the product was bad, but because no one modeled the messiness of healthcare data.”
Interoperability is not a feature you bolt on. It’s the backbone of the product.
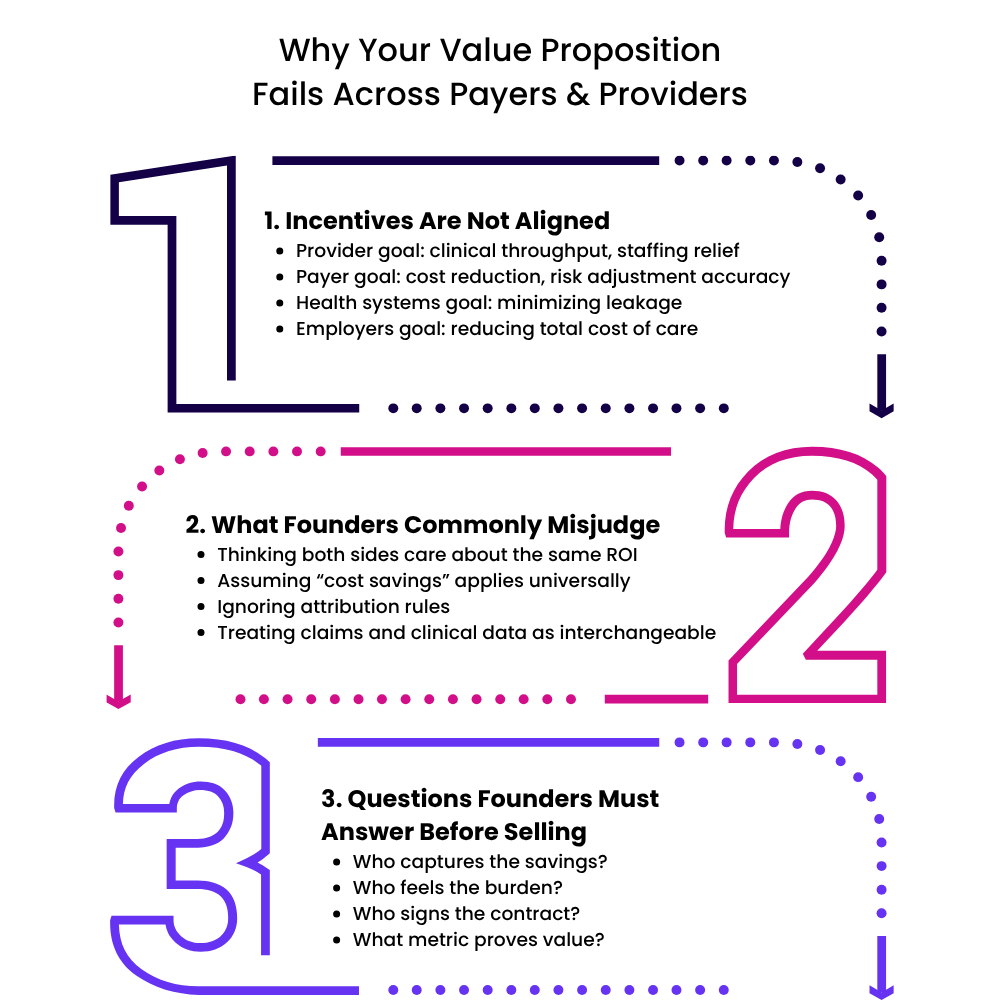
2. Oversimplifying Payer and Provider Dynamics
In 2026, payer and provider incentives are diverging faster than founders expect.
A workflow that improves physician efficiency may create zero value for a payer.
A solution that reduces payer cost may increase provider burden.
Founders fail when they:
- Pitch the same message to both sides
- Ignore attribution rules in value care
- Misunderstand prior authorization complexity
- Treat claims and clinical data as interchangeable
- Assume “cost savings” translate to “buying authority”
What I observed:
“A founder once asked me why a provider group wouldn’t buy their solution even though it reduced denials by 15%. The reason was simple: the payer, not the provider, captures that benefit. The founders didn’t map the incentives.”
A healthcare product is built after understanding who loses, who wins, and who decides.
3. Jumping Into AI Without Semantic or Regulatory Foundations
AI isn’t the problem. Shallow AI is.
Startups jump into:
- LLMs without ontology alignment
- Predictions without explainability
- Workflows without clinical guardrails
- Automation without audit trails
- Patient AI without regulatory clarity
By mid-2026, CMS, ONC, and HIPAA enforcement bodies will scrutinize:
- Model provenance
- FHIR semantics alignment
- Bias controls
- Safety layers
- Traceability of clinical recommendations
Without these, AI becomes a liability, not an advantage.
A lesson from the field:
“We saw a startup build an AI triage layer that looked fine in demos. But they had no ontology mapping. It classified ‘chest tightness’ as an ENT symptom. They didn’t need more AI. They needed clinical semantics.”
The winners in 2026 will be companies that build semantics and regulation, not demos.
4. Ignoring Compliance, Outcomes Attribution, and GTM
Compliance and GTM are not “business hygiene.” They are existential.
Startups fail when they:
- Build roadmaps without HIPAA, SOC2, HITRUST timelines
- Ignore FHIR mandates coming from CMS and ONC
- Promise value without a attribution methodology
- Run pilots without a outcomes framework
- Price the product without aligning to ROI triggers
In 2026, buyers are done experimenting. They want:
- Compliance posture
- Proof of clinical or operational lift
- Integration effort
- Pricing logic
Founders who skip these steps end up in “pilot purgatory”: an loop of demos, unpaid trials, and stalled contracts.
5. Weak Workflow Integration and No Investment in Data Engineering Patterns
Workflow is destiny. If clinicians can’t use it, no one will buy it.
Mistakes:
- Deploying solutions outside the physician’s workflow
- Not integrating with scheduling, ADT, or task queues
- Designing dashboards instead of decision supports
- Building custom ETL for every customer
- Not creating reusable ingestion, mapping, and QA patterns
The consequences are brutal:
- Integration timelines
- Deployments
- Analytics
- Onboarding
- Implementation costs
Founders realize this when scaling from 3 customers to 10, and everything breaks.
What I tell teams:
“Your product isn’t just the interface. Your product is the integration pathway, the data contracts, and the onboarding pattern. Miss that, and even a product becomes unscalable.”
The Way Forward: Discipline, Domain Fluency, and Automation
Avoiding these mistakes doesn’t require budgets. It requires thinking:
Build on domain fluency
Study incentives, governance, reimbursement, and clinical realities before building features.
Architect with interoperability first
Design FHIR schemas, clinical ontologies, and reusable ingestion pipelines from day one.
Make AI semantics
Ground every model in coded data, evidence pathways, and regulatory safety layers.
Create GTM that is evidence
Define outcomes, attribution logic, ROI triggers, and buyer incentives before launching your pilot.
Automate with responsibility
Use automation to eliminate tasks, not decision-making without safeguards.
Final Word
2026 will be unforgiving for healthcare startups that rush, improvise, or build in isolation from the ecosystem. But it will reward founders who combine technical execution, regulatory maturity, data discipline, and workflow sensitivity.
Healthcare doesn’t punish lack of innovation. It punishes lack of readiness.
Founders who understand this will not just survive 2026. They’ll build the next generation of healthcare companies.



