Why FHIR Alone Cannot Deliver Interoperability
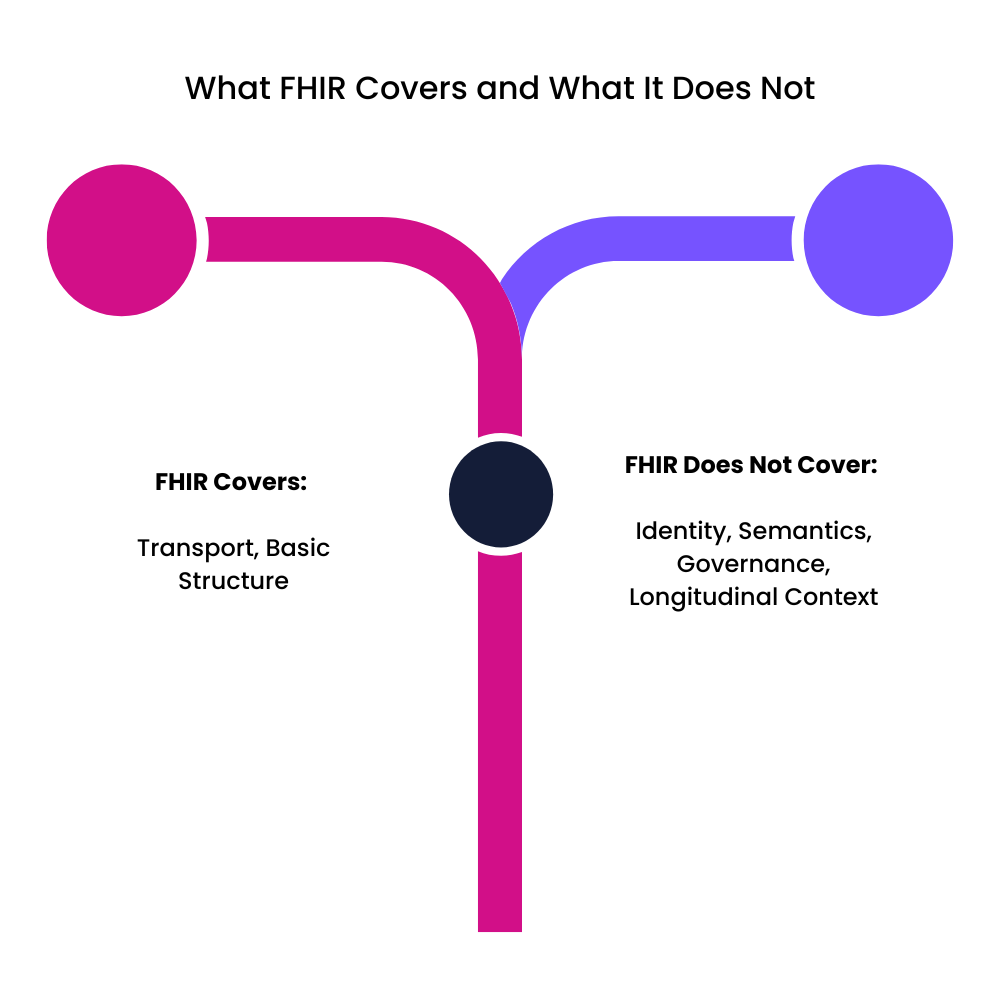
Healthcare leaders often assume that adopting FHIR APIs will unify their systems. But FHIR only solves transport, not meaning, identity, or continuity. True interoperability requires more than endpoints.
FHIR resources vary by vendor. Fields may be missing or coded differently. Identity mismatches break continuity. And most important, FHIR does not impose workflow, context, or data quality standards.
Common Gaps When Organizations Rely Only on FHIR
1. Inconsistent Implementation
Vendors choose which fields to support. This creates structural mismatches.
2. Missing or Partial Data Elements
Some systems send only minimal clinical or administrative fields.
3. Semantic Differences
The same clinical concept may be coded differently across systems.
4. Identity Fragmentation
Patient IDs differ across networks, breaking the record.
5. Limited Historical Depth
FHIR often exposes snapshots rather than complete histories.
Layers Required Beyond FHIR
1. Identity Resolution
Match patients across EHRs, labs, claims, and portals.
2. Terminology Mapping
Normalize LOINC, SNOMED, ICD, and CPT codes.
3. Data Normalization
Resolve duplicates, combine events, and standardize timestamps.
4. Governance
Establish rules for access, lineage, quality, and retention.
5. Context-Aware Enrichment
Add meaning through sequencing and clinical context.
These layers convert FHIR from a transport mechanism into part of a unified architecture.
Read the full whitepaper to understand the architecture behind real-time harmonization and longitudinal records.




