Who Actually Needs Longitudinal Patient Records in 2026?
We’ve been talking about unified patient records for a decade now. HL7 this, FHIR that, interoperability mandates, TEFCA frameworks. The infrastructure has been slowly coming together. But here’s what’s changed: in 2026, having fragmented patient data stops being “annoying but manageable” and starts being an actual business problem you can’t afford to ignore.
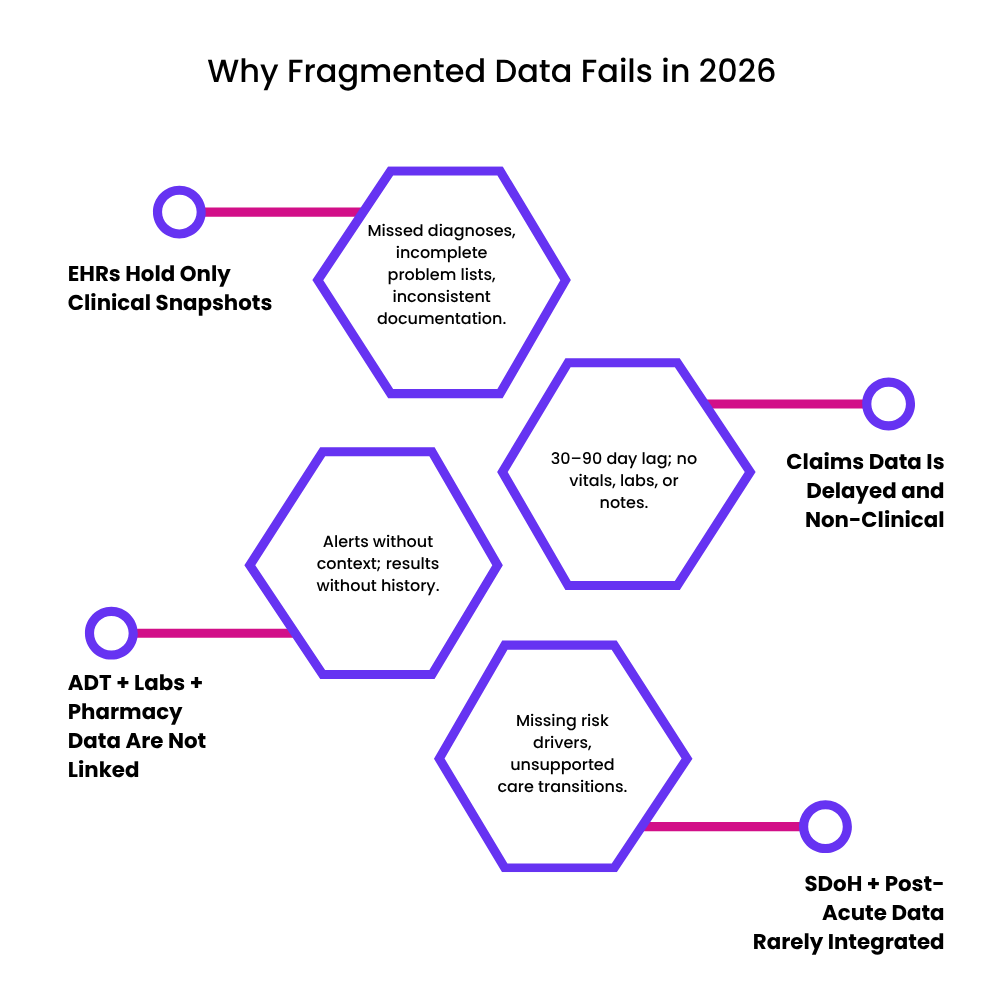
Think about where patient information lives right now. It’s everywhere. Your EHR has some of it. Claims systems have another piece. ADT feeds, lab systems, pharmacies, post-acute platforms, behavioral health records, social determinants data. Each one holds a chapter of the patient’s story, but nobody has the whole book.
And that’s killing you in ways you might not fully realize yet. Care quality suffers. Risk scores are wrong. Care coordination is guesswork. Reimbursement gets messed up. Clinical outcomes lag.
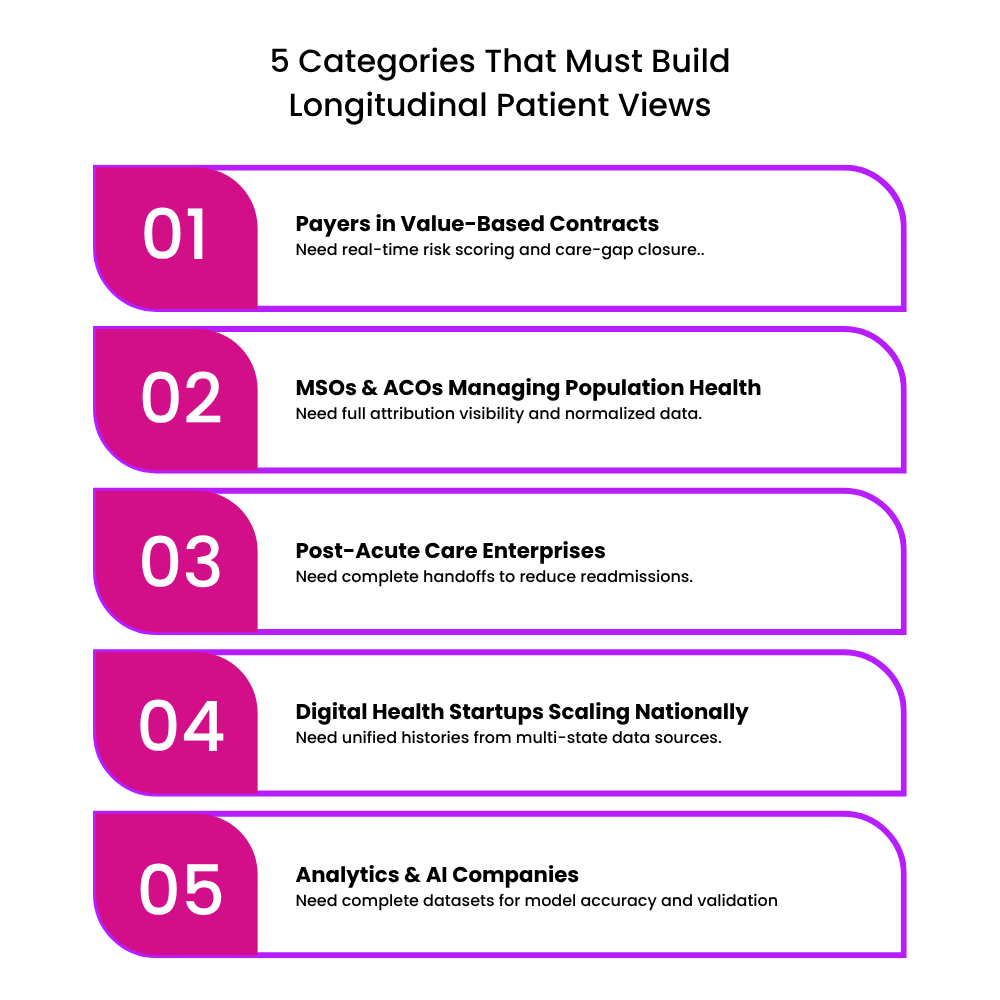
A Longitudinal Patient View (let’s just call it LPV) is basically a continuously updated, normalized record that pulls together all these scattered pieces. And in 2026, five types of organizations are going to feel the pressure to build this more intensely than anyone else.
1. Payers Running Value-Based Contracts
If you’re a payer getting into value-based care (or expanding what you’re already doing), you can’t work with partial information anymore. Your risk adjustment, HEDIS scores, care gap identification, network performance monitoring… all of it depends on having the complete picture, clinical and claims together.
Why this matters now:
Risk scoring needs current clinical data, not claims from a year ago. You can’t accurately assess someone’s risk profile when you’re working with stale information.
Network management requires catching high-risk events early. By the time you see it in claims, it’s too late to prevent anything.
HEDIS and Stars performance depends on pulling data from multiple systems and actually understanding what’s missing. You need to infer gaps, not just count what you can see.
CMS and state regulators are increasingly expecting you to show your work. Data transparency and evidence-based interventions aren’t nice-to-haves anymore.
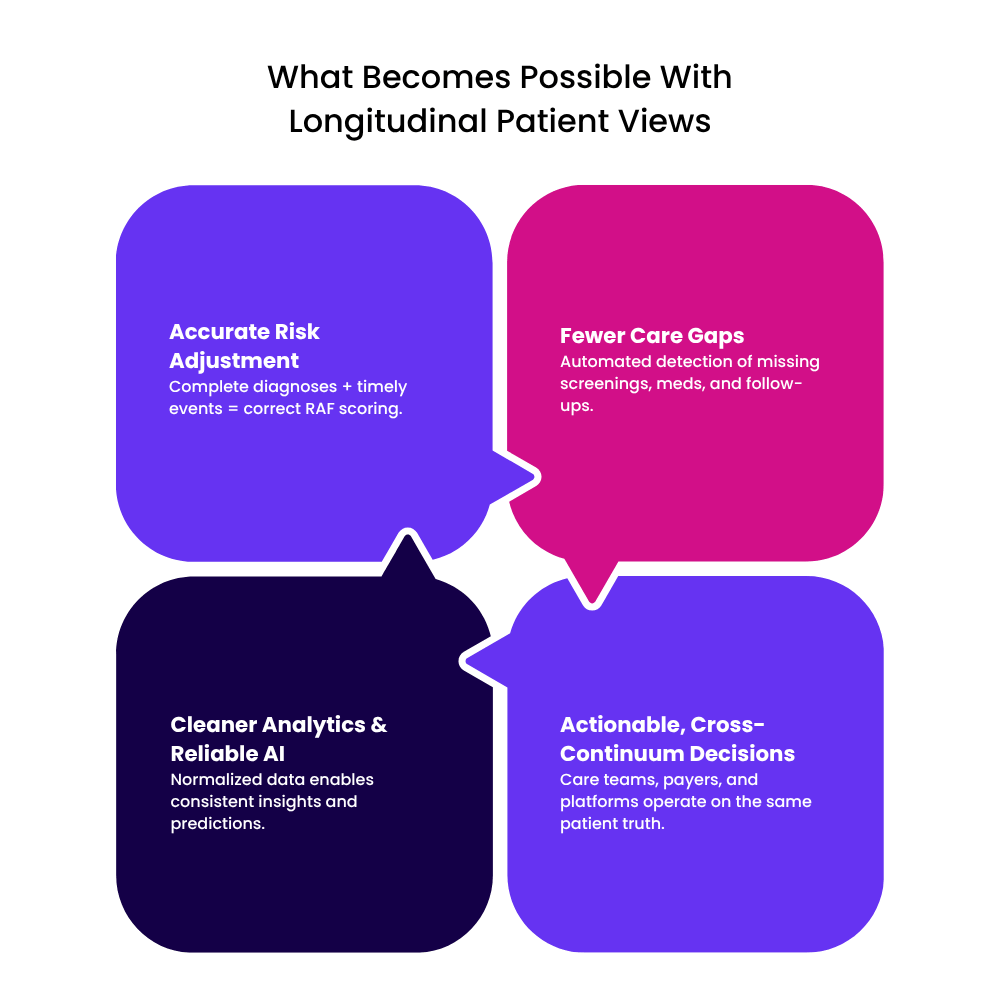
What you can actually do with an LPV:
Imagine combining ADT feeds with pharmacy data and prior auth activity in real time. You start seeing patterns before someone ends up in the hospital unnecessarily. Your risk models get better. Your care managers finally get one consolidated member record instead of having six tabs open trying to piece things together.
2. MSOs and ACOs Managing Populations
If you’re an MSO or ACO accountable for outcomes across a bunch of different provider groups, fragmented data is probably your biggest operational headache right now.
Why you need this:
The people you’re responsible for get care all over the place, often in systems you don’t control. Your population health insights are only as good as your data, and right now that data is arriving late, incomplete, and from a dozen different places that don’t talk to each other.
Care coordinators shouldn’t have to chase down charts manually. That’s not where their time should go.
What changes with an LPV:
You can automatically spot when chronic conditions are misclassified. Close screening gaps faster. Track transitions of care without waiting for faxes (yes, faxes) or making phone calls to track someone down. Your predictive models start reflecting reality instead of whatever partial data you managed to collect.
3. Post-Acute Providers Dealing With Transitions
Skilled nursing facilities, rehab centers, long-term care, home health agencies… you operate at the most vulnerable point in healthcare: when patients are moving between settings.
Why this is critical:
Patients show up with incomplete discharge information. Medication histories are missing or wrong. You’re flying blind at exactly the moment when the risk is highest.
Readmissions kill you financially and clinically, and a huge chunk of them happen because post-acute coordination falls apart.
Payers and hospitals want real-time updates for bundled payments and episode-based reimbursement. You need to deliver that or risk losing contracts.
What an LPV enables:
When someone arrives at a home health agency, they come with a complete handoff. Problem lists, recent imaging, pending labs, risk indicators, all of it. Immediately. That means fewer medication errors, faster care planning, and fewer readmissions that mess up your performance metrics.
4. Digital Health Companies Scaling Nationally
If you’re a digital health startup (virtual care, remote monitoring, chronic disease management, behavioral health, hybrid models), you hit a data wall when you try to scale beyond your initial region.
Why this becomes urgent:
Patients join your platform with histories from different EHRs. Some have been in three health systems. Some have moved states. Their data is inconsistent and incomplete.
Your clinical decision rules need normalized lab values, vitals, medication lists. Without that, your algorithms are guessing.
National expansion means dealing with hundreds of different data sources that all format things differently.
What becomes possible:
A diabetes management platform can automatically pull in and align A1c results, medication changes, hospitalization alerts from anywhere. Your clinicians and coaches see one coherent patient history regardless of where the data came from. You can actually scale without sacrificing quality.
5. Analytics and AI Companies Building Clinical Tools
Here’s the hard truth about AI in healthcare: your model is only as good as your data. If you’re feeding it fragmented, incomplete, inconsistently structured patient data, even the most sophisticated algorithm will give you garbage output.
Why LPV is foundational:
Those LLM-based clinical copilots everyone’s building? They need consistent, longitudinal context or they hallucinate. They make things up. That’s not acceptable in healthcare.
Risk models fall apart when diagnosis codes and lab values are missing or wrong.
Predictive algorithms depend on understanding how things change over time. You can’t do that with snapshots.
What this unlocks:
Analytics teams can finally run cohort analyses using complete patient timelines. AI recommendations become reliable because they know about recent medication changes, procedures, overlooked risk factors. Meeting regulatory requirements for explainability and data lineage gets a lot easier.
Why 2026 Is Different
Across all five of these categories, the same pressures are converging to make unified patient records urgent:
Operationally: Care teams are drowning in manual data reconciliation. It’s unsustainable.
Financially: Missed risk scores and unmanaged care gaps are costing real money. The penalties are getting bigger.
Regulatory: CMS, ONC, and payers are tightening requirements for data access and transparency. You can’t wave this off anymore.
Clinically: Fragmentation leads to misdiagnoses, duplicate tests, and avoidable bad outcomes. That affects both quality scores and, you know, actual human beings.
The Bottom Line
As we head into 2026, healthcare leaders have a choice. You can keep operating with incomplete visibility and absorb the growing costs and penalties. Or you can invest in building complete, longitudinal patient views that actually give you a competitive advantage.
The organizations that figure this out will have cleaner analytics, accurate risk adjustment, fewer care gaps, and more confident decision-making across the entire care continuum.
The ones that don’t? They’ll keep playing catch-up while their competitors pull ahead.
At TechVariable, we’re helping organizations across all five of these categories build LPV capabilities that actually work at scale. Not pilots. Not proofs of concept. Real systems handling real patient data in production. If you’re wrestling with this, let’s talk.