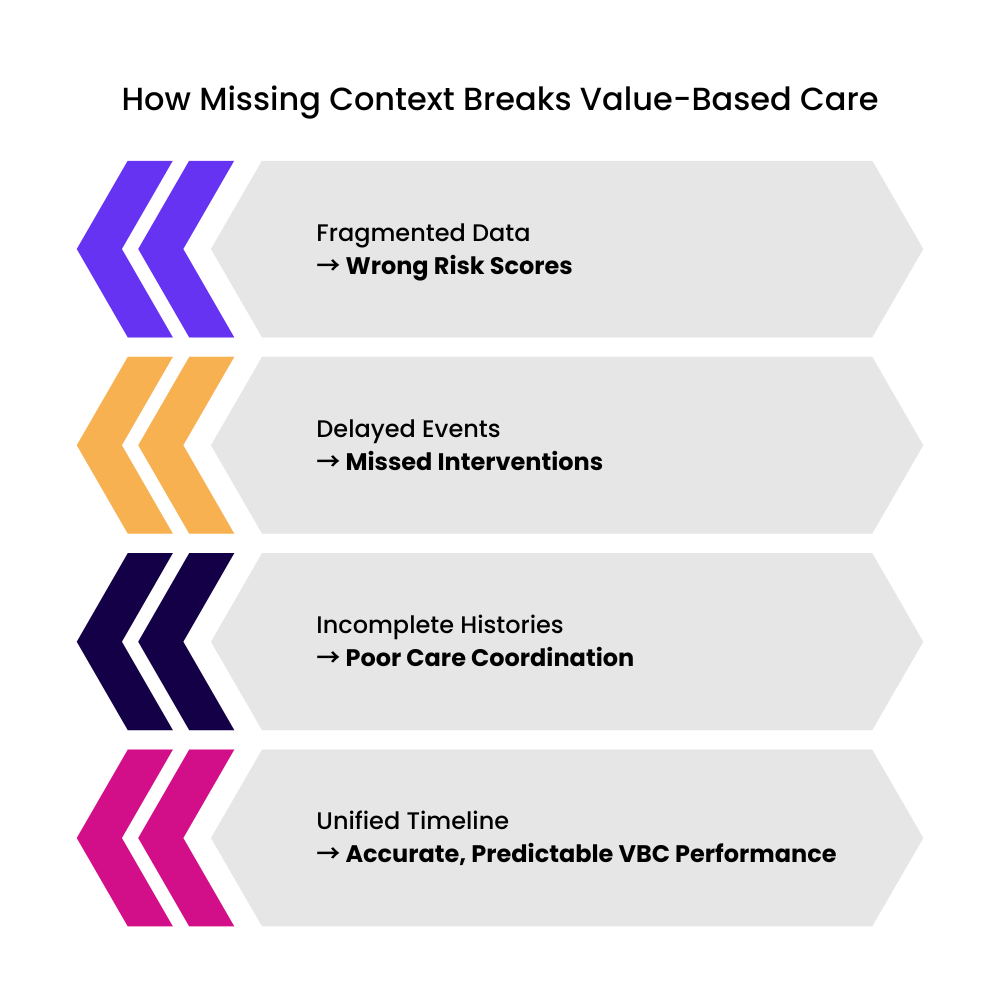
Why Value-Based Care Struggles in a Fragmented Data Environment
Value-based care rewards better outcomes and lower costs. Yet many organizations miss performance targets even when care teams work hard to close gaps. The core issue is not intention or clinical skill. It is the lack of complete and continuous patient records.
A patient’s history is often scattered across claims, EHRs, labs, and external providers. When information arrives late or incomplete, care teams work without context. This leads to preventable errors, reactive care, and inaccurate reporting.
How Missing Context Derails VBC Performance
1. Misaligned Incentives from Partial Data
Quality programs rely on accurate tracking of screenings, chronic conditions, and follow-up care. When half of the patient’s journey sits outside the local system, metrics appear worse than they are.
Examples include:
A cancer screening completed at an external facility that never reaches the primary provider
A chronic condition coded in claims but not reflected in the EHR
A behavioral health visit missing entirely from the clinical view
The result is underreported quality scores and reduced shared savings.
2. Delayed Data That Arrives After the Window Closes
Claims often come in weeks after the actual service. Lab data may arrive through PDFs. Hospital event alerts may fail to trigger real-time actions.
These delays lead to:
Late outreach to high-risk patients
Missed transitional care opportunities
Inaccurate risk models
VBC demands timely action but fragmented data works against this goal.
3. Incomplete Insights That Distort Clinical Decisions
Clinicians often lack visibility into:
Historical medication adherence
Behavioral patterns related to chronic conditions
Therapy response over time
Care plans become episodic rather than continuous.
What a Unified Longitudinal Record Changes
A longitudinal record connects every data point across time. It builds a single view from all sources including EHR, claims, labs, imaging, ADT feeds, care management notes, and device data.
This continuity enables:
Accurate identification of risk
Coordinated follow-up across teams
Timely gap closure
Reliable reporting for payers
Predictable financial performance
Longitudinal context turns fragmented information into a coherent story.
A Practical Roadmap to Build Longitudinal Patient Records
1. Ingest and Reconcile All Major Data Streams
Start with EHR, claims, and ADT feeds. Match patient identities and reconcile duplicates.
2. Normalize Data Into Standard Models
Use FHIR, LOINC, and SNOMED so data from different systems can align.
3. Add Time Sequencing and Context
Organize records by event timelines to reveal cause and effect.
4. Build Role-Based Views for Care Teams
Care managers, clinicians, and analysts should see the same patient view filtered to their workflow needs.
5. Establish Governance and Observability
Track data lineage, quality, and access to maintain trust.
To explore the full framework behind longitudinal data and VBC success, read the complete whitepaper.




